Osteoarthritis of the Knee
General Information about non-surgical management
This is a general information pack which is presented to all patients attending the Physiotherapy Osteoarthritis Class at Broadgreen Hospital and has been prepared by Jill Pope, Senior Physiotherapist.
Introduction:
Osteoarthritis (OA) is a progressive, degenerative process primarily affects weight bearing joints. It is the most common form of arthritis with over 7 million people suffering from osteoarthritis in the UK.
It can be classified as either Primary OA with no obvious cause or Secondary OA which may be due to a number of factors including poor lower limb biomechanics, deformity, previous trauma or infection.
There are a number factors which influence OA including activity, weight, diet, climate and humidity.
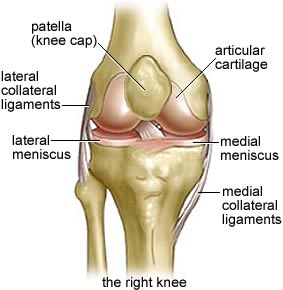
Changes in Osteoarthritis:
A number of changes occur within the joint including:
- Reduced cartilage thickness
- Decreased joint space
- Osteophytic (bony spurs) formation
- Loose bodies
- Thickened or inflamed joint lining
- Irregular joint surface
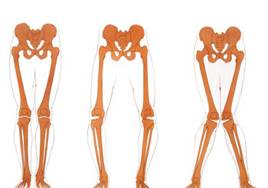
These result in a number of signs and symptoms including pain, stiffness, reduced range of movement, joint swelling, muscle wastage, joint clicking, reduced function and mobility and deformity. The deformity can be either ‘bow-legging’ (varus) or ‘knocked knees’ (valgus) depending which side of the joint is most affected.
Baker’s Cyst:
A Baker's cyst is an accumulation of joint fluid (synovial fluid) that forms behind the arthritic knee. It is most often painless but can occasional cause discomfort. It feels like a water-filled balloon. Occasionally, the cyst may rupture, causing pain, swelling, and bruising on the back of the knee and calf. Often no treatment is necessary and a GP can observe the cyst over time. If the cyst is painful, treatment is usually rest, ice, anti- inflammatories.
Removal of the cyst is generally not done because it will accumulate through the arthritic knee and there is a small risk of damage nearby blood vessels and nerves. It is remioved when a totoal knee replacement is undertaken. Rarely a cyst can be drained (aspirated), if the fluid inside it has become solid and gel-like.
Role of Physiotherapy:
Physiotherapy helps with self management and education in arthritis to improve and maintain joint movement, control swelling, improve and maintain muscle power, minimise joint damage and maximise mobility and function. The treatment options include exercise, stretches, joint mobilisation, heat packs, ice packs, electrotherapy such as TENS and acupuncture. Orthotics and other aids may help such as walking aids, insoles, footwear, shoe raises and knee supports.
Medication:
There are a number of various drugs that can help. It is important to discuss these with your general practitioner or surgeon, as not all are suitable for all patients. The various groups include:
- Analgesic e.g. paracetamol, co-codamol
- NSAIDs e.g. ibuprofen, arthrotec, diclofenac
- Supplements e.g. glucosamine, chondroitin sulphate
- Injections e.g. dexamethasone (DMI)
-
Glucosamine is currently well marketed and claims to be a joint lubrication and cartilage-building nutritional supplement that helps damaged joints, tendons, cartilage and soft tissue. It is a naturally occurring substance which is found in the body, primarily in cartilage and synovial fluid. It may help the pain and stiffness in your knee. The recommended dosage for glucosamine is 1,500mg per day which can be taken as one 1,500mg dose, two 750mg doses or three 500mg doses. The effects of glucosamine normally take about four weeks to be realised and it is important to realise that it is not an instant action supplement. The scientific evidence for and against its efficacy, however is poor and so if there is no change after 4 months it is probably not worth taking it. As with any medication, check with your GP before starting it.
Diet & arthritis:
Evidence shows that excessive weight and the type of diet you follow may influence your knee pain. We can all benefit from eating a healthy, well-balanced diet. The World Health Organization recommends that we eat at least five portions of fruit and vegetables every day; switch from white to whole-grain products; and reduce sugar, salt and saturated fat found in animal products. Other foods such as Omega-3 oils particularly as found in oily fish can be helpful to control inflammation. These are ONLY found in anchovies, eel, herring, kippers, mackerel, pilchards, salmon, sardines, sprats, swordfish, trout, tuna (fresh not tinned) and whitebait. It is probably a good idea to eat oily fish twice a week. It is important not to confuse this with fish liver oil (cod liver oil) It is dangerous to take fish liver oils in the large doses recommended for arthritis because of the risk of overdosing with vitamin A. If you feel that you need an individual dietician assessment please let the physiotherapist know at the end of the session or ask your GP to refer you.
Physiotherapy Excersises:
These include a number of excersises including:
- Quadriceps-SLR
- Hamstrings- standing hamstring curls
- Sit/stand from chair
- Step ups on a small step
- Balancing one leg
- Exercise bike
- Lower limb stretches
It is important to maintain, if possible, general exercise such as swimming, cycling and walking.
Self management of your arthritis during acute flare ups include RICE (rest, ice and elevation), increasing analgesics (check the maximum dose) and a gradual return to normal activity. Physiotherapy can help limit deterioration with a combination of helping avoid painful prolonged positions, walking aids, avoidance of high impact activities, avoidance of loading with rotation and with joint protection e.g. kneeling pads.
Summary:
Osteoarthritis (OA) is a progressive, degenerative process primarily affects weight bearing joints. It is the most common form of arthritis with over 7 million people suffering from osteoarthritis in the UK. Its non-surgical treatment is based around learning how to manage acute flare up, picking the right activities, keep moving - little and often, balance activity with rest and finally, seek help if necessary.